Key Takeaways
Plantar fasciitis is a common cause of heel pain, especially with your first steps after waking or sitting for long periods
Stretching, rest, ice, and supportive footwear can ease symptoms and help prevent chronic issues when started early.
Persistent plantar fasciitis symptoms often require a podiatrist’s expertise to guide treatment, from conservative therapies to more advanced procedures.
Plantar fasciitis is a common cause of heel pain. Up to 1 in 10 people experience plantar fasciitis during their lifetime. Symptoms range from mild to severe. This condition may affect your ability to walk and carry out daily activities.
The good news is that effective treatments are available. Some can be done at home. Physical therapy and a doctor’s care often help. Early treatment is important.
What Is Plantar Fasciitis?
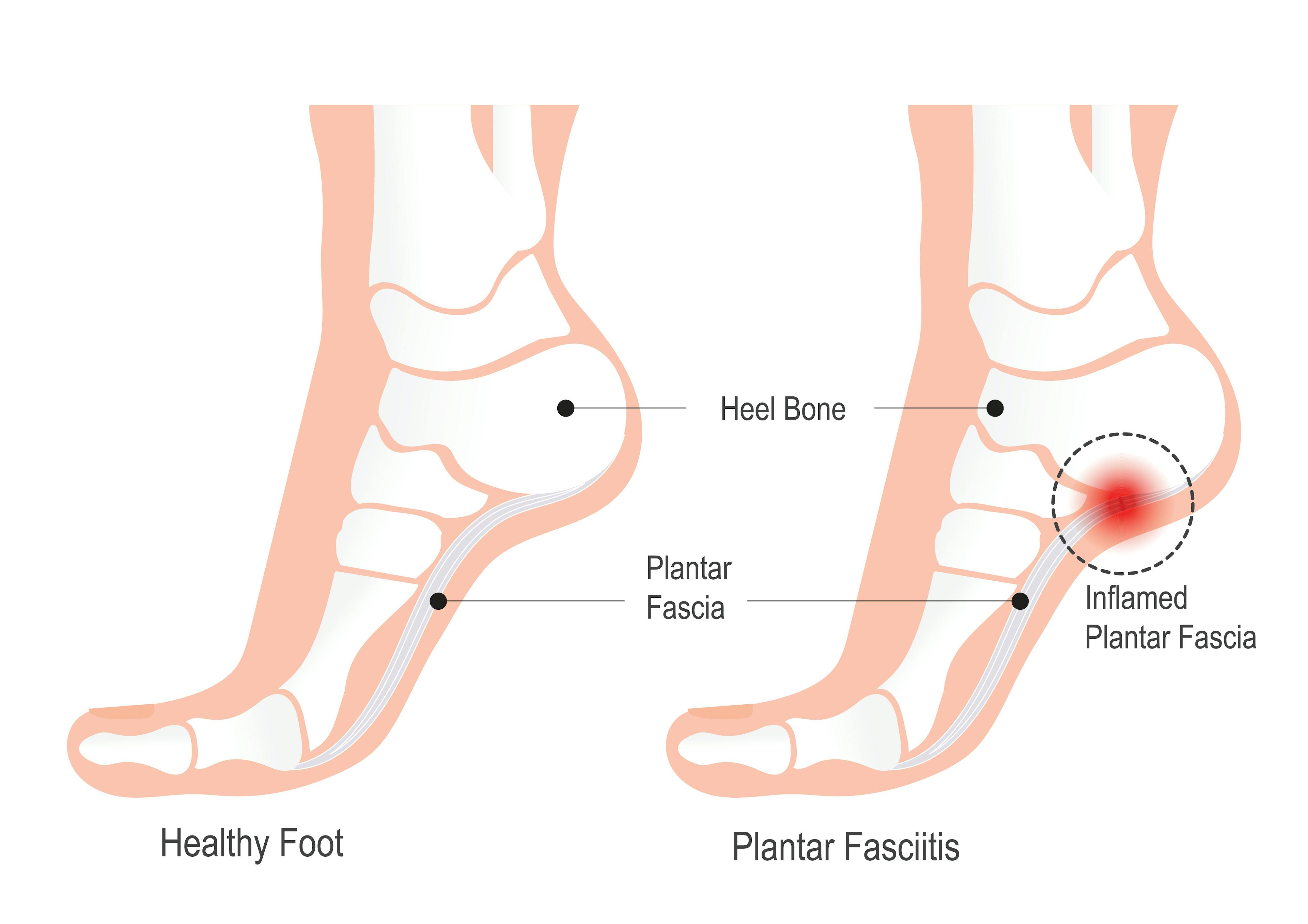
Plantar fasciitis (plan-ter fash-ee-ahy-tis) is a common condition causing heel pain, especially after resting or standing for a long time. It develops when the plantar fascia—a band of tissue on the bottom of the foot—becomes inflamed or injured. The pain occurs where the plantar fascia attaches to the heel bone or along its course in the arch of the foot and is often worst with the first steps in the morning or after periods of rest. This condition may affect your ability to carry out daily activities.
Plantar Fasciitis Symptoms
The key symptom of plantar fasciitis is a sharp, stabbing pain near the heel, especially with the first few steps in the morning or after a long rest. Your heel or bottom of the foot may be painful to the touch. The pain often worsens at the end of the day.
Causes of Plantar Fasciitis
You are more likely to get plantar fasciitis if you:
- Have foot arch problems (flat feet or high arches)
- Run long distances, downhill, or on uneven surfaces
- Are overweight or have a sudden weight gain
- Boost your activity level (like starting a walking or running program)
- Have a tight calf muscle or limited ankle flexibility
- Wear shoes with poor arch support or soft soles
- Stand for long periods
- Have a low-activity (sedentary) lifestyle
Plantar fasciitis is often linked with heel spurs, bony growths that develop on the heel.
Diagnosis of Plantar Fasciitis
Usually, your doctor diagnoses plantar fasciitis based on your symptoms and by checking your foot and ankle for swollen or painful areas.
Your doctor may order imaging tests, such as X-rays, magnetic resonance imaging (MRI), or ultrasound scans—especially for chronic (long-term) plantar fasciitis.
How to Treat Plantar Fasciitis
For some people, plantar fasciitis goes away without medical intervention, especially in early or mild cases. Early, consistent treatment—like stretching, rest, and supportive shoes—often leads to faster recovery. Most people begin to feel better within one to four weeks of starting consistent treatment.
Your local foot and ankle specialists can diagnose and treat plantar fasciitis. They offer care ranging from recommended stretches and orthotics (shoe inserts) to advanced treatments like injections or surgery, if needed.
Starting treatment early supports a faster healing process and lowers the risk of later complications, including chronic heel pain, an altered gait, or joint problems in other parts of the body.
Once your condition is under control, you can take steps to prevent future flare-ups.
At-Home and Conservative Treatments
Treatment often begins at home. Your doctor may recommend:
- Exercises to gently stretch the plantar fascia
- Calf stretching exercises
- Ice packs to reduce inflammation
- Nonsteroidal anti-inflammatory medicines (NSAIDs), taken as pills or as a gel to rub into your heel, as directed by your medical provider
- Supportive shoes to relieve strain on the plantar fascia
- Over-the-counter arch supports
Medical Treatments
If your symptoms do not improve or worsen, your doctor may recommend:
- Physical therapy to strengthen the foot and enhance mobility
- Custom orthotic shoe inserts
- Corticosteroid injections to relieve stubborn inflammation
- Iontophoresis, which uses a mild electrical current or a special patch to push medicines (like corticosteroids) through the skin to help relieve inflammation and reduce pain
- Alternative treatments including laser or photobiomodulation therapy (PBMT), shockwave therapy, and platelet rich plasma (PRP) may help the healing process
Surgical Treatment Options
Surgery is typically considered only in advanced or chronic cases when conservative treatments have not provided relief and heel pain continues to interfere with daily life. Surgical options may include minimally invasive procedures or traditional plantar fascia release, depending on the severity of tissue damage and patient goals. To better understand how modern minimally invasive techniques compare to open surgery, explore our detailed guide on Tenex vs. traditional plantar fasciitis surgery.
When to See a Podiatrist
If heel pain continues despite rest and conservative care, or if it begins to interfere with your daily activities, it may be time to seek professional evaluation. A podiatrist can help identify any contributing issues and recommend a tailored approach based on your needs. Early intervention may shorten recovery time and help prevent long-term discomfort or mobility problems.
FAQs
In many cases, plantar fasciitis goes away with early, consistent treatment under the guidance of a podiatrist.
The key symptom is a sharp, stabbing pain near the heel, especially with the first few steps in the morning or after a long rest. Your doctor may order tests to rule out other causes of foot pain.
Although exercises can provide relief from uncomfortable symptoms, some cases require professional treatment beyond at-home care or the expertise of a primary care provider.
If you experience the following, it may be time to consult a podiatrist:
- Persistent or worsening heel pain
- Trouble walking or standing for long periods
- Pain that hasn’t subsided after several weeks of stretching
Plantar fasciitis causes a sharp, stabbing pain near the heel. The pain is usually worse when you take a few steps after waking up or after a long rest. You may feel pain when pressing on your heel or while walking. Symptoms are often worse at the end of the day.
To help relieve your symptoms and promote recovery from plantar fasciitis, your doctor may recommend:
- Exercises to gently stretch the plantar fascia
- Calf stretching exercises
- Ice packs to reduce inflammation
- Nonsteroidal anti-inflammatory medicines (NSAIDs), taken as pills or as a gel to rub into your heel, as directed by your medical provider
- Supportive shoes to relieve strain on the plantar fascia
- Over-the-counter arch supports