Permanent Male Birth Control
Every year, approximately 500,000 men in the U.S. choose to get a vasectomy.
This is largely due to the procedure’s high success rate of nearly 100% as a form of permanent male birth control.
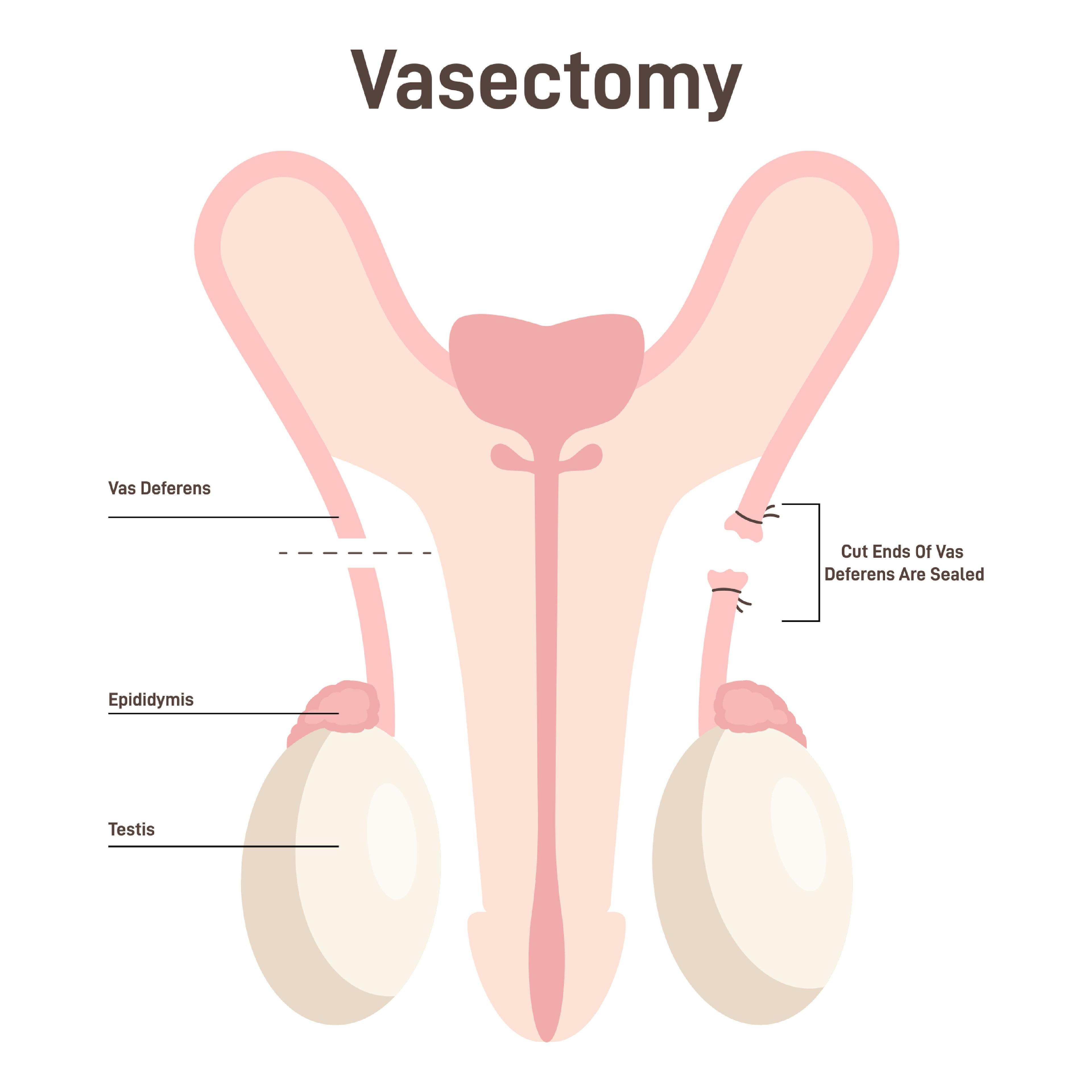
A vasectomy prevents the release of sperm into the ejaculate by interrupting the vas deferens, the ducts that transport sperm. This procedure can be performed using various techniques, each tailored to prioritize safety and minimize discomfort.
Both methods are highly effective as permanent birth control solutions, with the main differences being the surgical technique and recovery process.
Traditional Vasectomy
This method involves a small incision made in the scrotum to access the vas deferens, which are then cut and sealed. Vasectomies are highly effective with a 99% success rate in preventing pregnancy. The recovery time is minimal, typically requiring just a few days of rest and avoidance of strenuous activities.
No-Scalpel Vasectomy
The no-scalpel vasectomy is a minimally invasive procedure that eliminates the need for an incision. Instead, a small puncture is made to access the vas deferens, which reduces the potential for complications and discomfort.
This method also offers a quicker recovery time and is generally less painful compared to the traditional approach.
What Happens During a Vasectomy?
Understanding what happens during the procedure can help ease any anxieties and prepare you for the experience. Here is a step-by-step overview of what typically occurs during a vasectomy:
Before the vasectomy, you will have a consultation with your CLS Health urologist to discuss the procedure, its risks, benefits, and any questions you may have. On the day of the procedure, you will be advised to shave the scrotal area and thoroughly clean it.
The procedure begins with the administration of a local anesthetic to numb the scrotum, as this ensures that you remain awake but free of pain during the vasectomy. You may feel a brief sting or pinch as the anesthetic is injected.
There are two common methods for performing a vasectomy:
- Traditional Method: The surgeon makes one or two small incisions in the scrotum to access the vas deferens, the tubes that carry sperm from the testicles to the urethra.
- No-Scalpel Method: The surgeon makes a tiny puncture hole in the scrotum using a special instrument. This method tends to cause less bleeding and fewer complications than the traditional method.
Once the vas deferens are accessed, the surgeon will:
- Cut each tube.
- Seal the ends by tying them, using surgical clips, or cauterizing (burning) them.
- In some cases, a small section of the vas deferens may be removed.
This process prevents sperm from mixing with the semen that is ejaculated, thereby preventing pregnancy.
For the traditional method, the small incisions are usually closed with dissolvable stitches. In the no-scalpel method, the puncture hole is so small that it typically heals without the need for stitches.
After the vasectomy, you will be given post-procedure care instructions, which typically include:
- Rest, take it easy for the next few days. Also, over-the-counter pain relievers can help manage any discomfort.
- Apply ice packs to the scrotal area to reduce swelling and discomfort.
- Wear snug underwear or a jockstrap to provide support and minimize movement of the scrotum.
Ready to Take the Next Step? Schedule Your Vasectomy Consultation in Houston Today.
Choosing a vasectomy is a personal and proactive decision for your future. Our experienced urology team provides safe, confidential, and compassionate care every step of the way. If you’re ready to explore your options or have questions about the procedure, we’re here to help. Book your consultation today and take control of your reproductive health with confidence.
Find a Urologist Near You

Urology

Urology

Urology
FAQs
Ideal candidates for vasectomy are men who are certain they do not want more children and are looking for a reliable, permanent form of contraception, also, these procedures are suitable for those seeking less invasive options with minimal recovery times. It’s important to have a thorough discussion with your urologist to understand the permanent nature of the procedure and ensure it aligns with your long-term family planning goals.
Both traditional and no-scalpel vasectomies typically cause minimal discomfort. The no-scalpel vasectomy is especially known for its reduced pain, as it does not involve an incision; only a small puncture that may feel like a mosquito bite during the anesthetic application. Most men report feeling some pressure or mild discomfort during the procedure, but this is generally well-tolerated.
Vasectomy recovery time usually involves a few days of rest and most men can resume normal activities within a week. It is advisable to avoid strenuous activities and sexual activity for about 7 to 10 days to ensure proper healing. Also, applying ice packs and wearing supportive underwear can help reduce swelling and discomfort during the initial recovery period.
Long-term side effects are rare for both types of vasectomy, and any persistent pain or complications should be discussed with your urologist. However, a small number of men may experience chronic discomfort or develop post-vasectomy pain syndrome, though these complications are uncommon. Short-term side effects might include swelling, bruising, and minor pain, which typically resolve within a few days to weeks.
No, a vasectomy does not cause erectile dysfunction. The procedure does not affect hormonal levels, sexual drive, or the ability to achieve and maintain an erection. It solely prevents sperm from being present in the ejaculate, thereby preventing pregnancy.
While vasectomy reversal procedures exist, they are complex and not always successful. Therefore, vasectomy should be considered a permanent solution and men who are considering a vasectomy should be sure they do not want to father children in the future. Something to keep in mind when making this decision is that the success rate of reversal decreases the longer the time since the vasectomy.
You should continue using other forms of contraception until a semen analysis confirms the absence of sperm. This test is typically done several months after the procedure to ensure that sperm are no longer present in the ejaculate. It is crucial to follow up with your healthcare provider to schedule this test and confirm the effectiveness of the vasectomy.
The cost of a vasectomy in Houston can vary, generally ranging from $400 to $1,200. CLS Health urology clinics accept Medicare, as well as most major insurance plans. Many insurance plans cover the cost of the procedure, but it’s advisable to check with your insurance provider for specific details about coverage and any out-of-pocket expenses you may incur.