Diabetic foot ulcers are a common foot problem associated with diabetes. According to recent data, nearly one-third of type 2 diabetes patients may develop diabetic foot ulcers at least once in their lifetime.
Patients have a better chance of a full recovery when the ulcers are treated in the early stages. In the advanced stages, there’s a high risk of complications. This article covers the symptoms, stages, and treatment options for diabetic foot ulcers to help you make the most informed decisions about your foot care.
What Causes Diabetic Foot Ulcers?
Several risk factors increase the likelihood of developing diabetic foot ulcers. By managing these risk factors and working closely with your podiatrist, you can reduce the chances of developing a diabetic foot ulcer.
- Neuropathy
Diabetic neuropathy causes a loss of sensation in the feet, making it difficult to detect small injuries. When unnoticed, these minor injuries can worsen into ulcers. Motor neuropathy weakens foot muscles, leading to deformities like hammertoes that create pressure points, increasing the risk of ulcers. - Peripheral Artery Disease (PAD)
PAD occurs when blood flow to the lower limbs is reduced due to narrowed arteries. This poor circulation slows wound healing and increases the risk of ulcers and amputations. Symptoms of PAD, such as cramping or pain in the legs during activity, can progress to critical limb ischemia, which further increases the risk of ulceration. - Foot Deformities
Foot deformities like bunions, hammertoes, or collapsed arches cause abnormal pressure points on the foot, which can lead to ulcers. Wearing ill-fitting shoes can worsen these pressure points, making ulcer formation more likely. - High Blood Sugar Levels
Elevated glucose can impair the body’s ability to fight infection and heal wounds.
What Does a Diabetic Foot Ulcer Look Like?
Foot ulcers or diabetic foot sores, commonly occur on the bottom of the feet in people with diabetes. Foot ulcers may be surrounded by thickened, callused skin and can sometimes discharge pus or other fluids.
Diabetic Foot Symptoms
Symptoms of diabetic foot ulcers vary based on type. These are typical in the beginning stages:
- Cracks
- Dryness
- Redness
- Scaliness
- Rashes
These are common when the condition worsens:
- Pain or tenderness
- Swelling and inflammation of the ulcerated area
- A hard area at the center of the wound
- Skin discoloration
- Discharge of fluid or pus
- A foul smell
Diagnosis of Diabetic Foot Ulcers
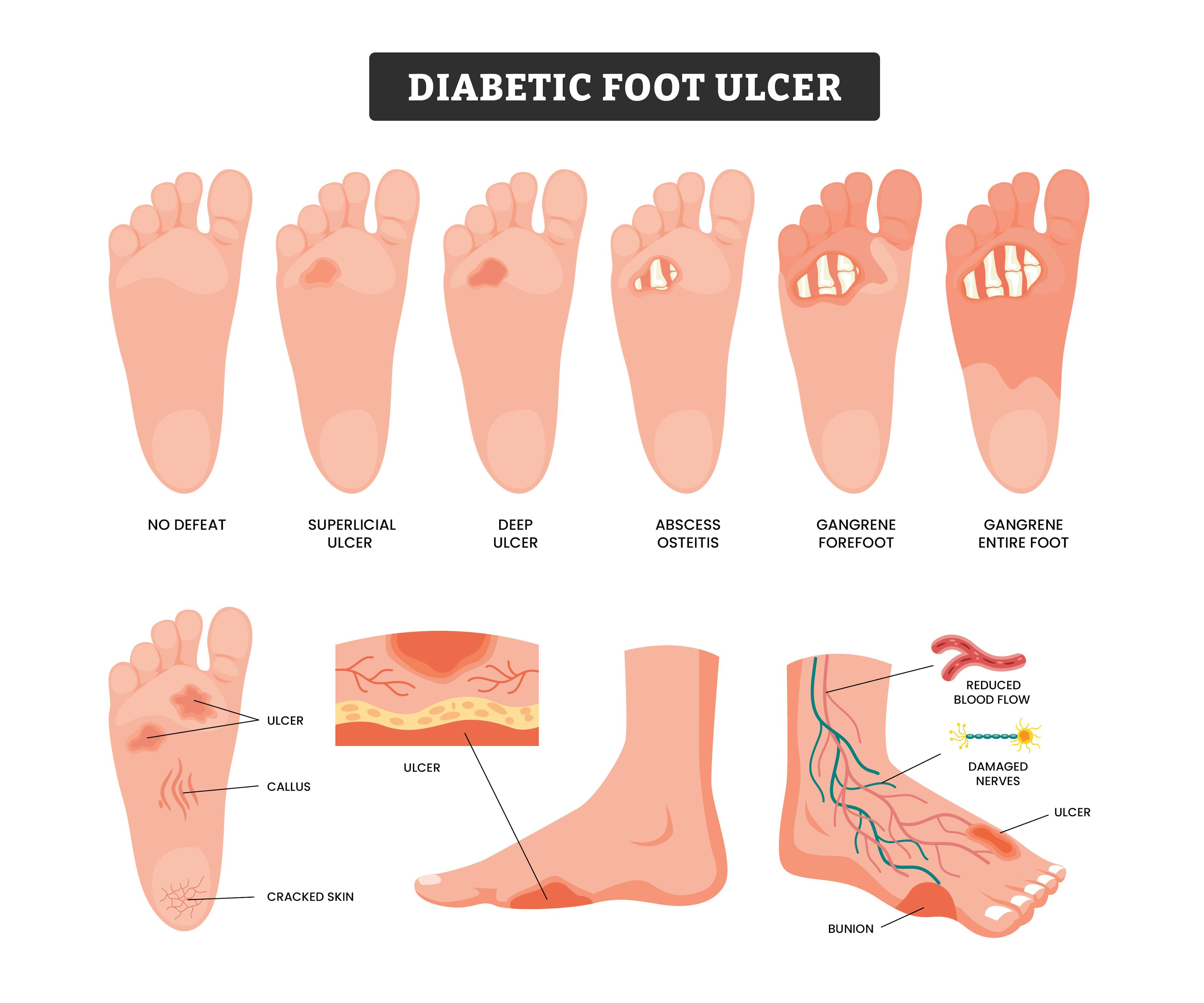
When evaluating diabetic foot ulcers, a foot specialist will usually begin by examining the size, depth, and location, along with the area affected. The doctor will also likely use the 6-stage Wagner Ulcer Classification System to assess the severity of the ulcer. Here’s a guide to help you understand the progression of these stages.
Diabetic Foot Ulcer Stages
Stage 1: No open ulcer, but foot is at risk due to deformities or healed previous ulcers.
Stage 2: A superficial ulcer affecting only the top layer of skin.
Stage 3: The ulcer extends deeper, reaching tendons, bones, or joints.
Stage 4: Deep ulcers with infection, possibly affecting the bone (osteomyelitis).
Stage 5: Gangrene (tissue death) in part of the foot, such as the toes or heel.
Stage 6: Extensive gangrene involving most or all of the foot.
Diabetic Foot Ulcer Treatment
Treating diabetic foot ulcers requires a combination of strategies to promote healing and prevent complications. Early treatment can help to avoid infections and more serious outcomes like amputation. Primary treatment approaches include:
- Off-loading: To reduce pressure on the ulcer, your doctor may recommend staying off your feet as much as possible. Special shoes, braces, or casts may also be used to relieve pressure from the affected area and allow the ulcer to heal.
- Debridement: This involves the removal of dead skin, foreign material, or infected tissue from the wound. Debridement can be done surgically, enzymatically, or using biological methods like maggot therapy to clean the wound and encourage healthy tissue growth.
- Infection Management: If the ulcer becomes infected, it is imperative to treat the infection promptly. Antibiotics may be prescribed based on the type of bacteria present, determined by lab testing. In some cases, intravenous (IV) antibiotics or hospitalization may be necessary for severe infections.
- Dressings and Wound Care: Keeping the wound clean and moist helps promote healing. Specialized dressings, such as calcium alginate or hydrocolloid dressings, are often used to absorb excess fluid, reduce bacterial growth, and protect the wound.
- Surgery: In severe cases, surgery may be needed to remove bone abnormalities or correct deformities like hammertoes or bunions that contribute to ulcer formation. If the ulcer causes significant tissue loss or a life-threatening infection, amputation may be the only option.
Prevention of Diabetic Foot Ulcers
If you’re at risk for diabetic foot ulcers, these are some proactive measures you can take to protect your feet.
- Visit Your Podiatrist Regularly: Regular checkups with a diabetic podiatrist are important for detection of potential complications. Your podiatrist can provide personalized prevention strategies.
- Wear Proper Footwear: Ill-fitting shoes can cause pressure points and friction, leading to ulcers. Make sure your shoes fit well and provide adequate support. Consult your podiatrist for recommendations.
- Inspect Your Feet Daily: Make it a habit to check your feet every day for cuts, blisters, redness, or cracks. Pay special attention to the soles and between your toes. If you spot anything unusual, schedule an appointment with your podiatrist promptly.
- Keep Your Blood Sugar Under Control: Managing your blood sugar is one of the most effective ways to prevent foot ulcers, as high blood sugar can hinder healing and increase the risk of infection.
- Reduce Lifestyle Risk Factors: Smoking, alcohol use, and high cholesterol can contribute to the risk of ulcers. Managing these through healthy habits can help safeguard your feet.
Need Diabetic Foot Care? Book a Specialist Visit.
Regular podiatrist visits are important for anyone with diabetes to avoid foot-related complications. Regardless of your health condition, it’s critical to contact a healthcare provider immediately if you find an ulcer on your foot or toe. Left untreated, it may become infected and lead to serious medical problems. Schedule a consultation with a diabetic foot specialist today.







